Platelet Count
Definition, Low vs Normal vs High, and RangesWhat does platelet count mean?
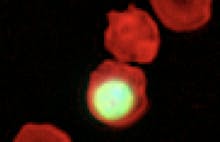
Platelets, also called thrombocytes, are small blood cells produced in the bone marrow. When a blood vessel is damaged, platelets clot together to effectively “plug” the injury and stop bleeding. A platelet count is a diagnostic test carried out to determine how many platelets are present in a patient’s blood.
Low platelet count or high platelet count can indicate disorders of the bone marrow.
What is a normal platelet count?
There are normally between 150,000–450,000 platelets in each microliter of blood.
What is a low platelet count?
A count lower than 150,000 platelets per microlitre of blood is considered to be thrombocytopenia, which means a lower than normal platelet count. Below 50,000 is a seriously low platelet count.
Below 10,000 is considered severe thrombocytopenia, with a risk of internal bleeding.
What is a high platelet count?
A platelet count above 450,000 platelets per microliter of blood is considered to be high. The technical name for this is thrombocytosis.
What does it mean when your platelet count is low?
If you have a low platelet count, then you have a condition called thrombocytopenia. This might be caused by a bone marrow disorder such as leukemia, an immune system disorder along with anemia (low hemoglobin count), or a viral infection such as hepatitis. Alternatively, thrombocytopenia can be a side effect of taking some medications such as chemotherapy or certain antibiotics that can interfere with the bone marrow .
Thrombocytopenia may be mild and a person may have no symptoms with it. However, a lack of platelets means that the blood may not clot properly. If it is a severe case, symptoms include increased bruising, heavy menstrual flows, blood in the urine or stool and bleeding gums. It can also cause a skin rash of superficial bleeding called petechiae, which looks like tiny red dots and can often appear on the lower legs.
What does it mean when your platelet count is high?
High platelet count can indicate either essential thrombocythemia or reactive thrombocytosis.
Essential thrombocythemia is a rare bone marrow condition which causes the body to overproduce platelets. This is a chronic condition and is caused by genetic mutation, but the reasons for this abnormality are uncertain.
Reactive thrombocytosis is a temporary elevation of the blood cells in response to another condition. While the response itself is often a normal part of acute inflammatory processes, reactive thrombocytosis can be caused by cancer, anemia or certain auto-immune disorders. It generally resolves when the underlying condition is treated.
Platelets are important for the body as they clump or stick together in response to injury and prevent excessive bleeding. However, an abnormally high platelet count means that clotting could happen spontaneously. Blood clots may occur anywhere in the body, but are most common in the hands, feet and brain. Other symptoms of high platelet count include headaches, dizziness, weakness and fainting.
How to increase platelet count?
There are a number of treatment approaches for an abnormally low platelet count. If the thrombocytopenia is not causing physical symptoms, treatment is usually not required.
However, if a low platelet count is dangerously low or symptomatic, then the cause may need to be treated directly. Since there is a wide range of possible causes, resolving thrombocytopenia often involves treating the underlying medical condition or switching medication.
For certain forms of thrombocytopenia, a doctor might prescribe drugs which suppress the immune system; a common medication used for this is the corticosteroid drug prednisolone.
Depending on the cause and if platelet count does not increase, the patient may undergo splenectomy: an operation to remove the spleen. The spleen is essentially a blood filter, but if functioning abnormally, can sometimes become overly destructive to platelets. Response to splenectomy can typically be an increase in platelet count of 30% to 100%.
In emergencies or for chronic and unremitting thrombocytopenia, patients with severely low platelet count or significant bleeding may be treated with blood or platelet transfusions.
What is platelet clumping?
Platelet clumping is a rare occurrence where platelets in a blood test sample stick together. This has no clinical relevance, but can result in a false low platelet count.
This false reading happens because most hematology analyzers count platelets by size.
The clump of platelets is too large to be recognized by the analyzer as made from platelets, so the analyzer is programmed to disregard them.
This results in a platelet count result which is lower than it actually is. This situation is sometimes referred to as pseudo thrombocytopenia.
Assessing platelet count for clinical trials
One of the adverse effects of some clinical trial drugs is very low platelet counts. Certain drugs destroy blood platelets or prevent the bone marrow from making normal amounts of platelets.
Clinical trial drugs are usually administered in Phase I-IV trials, and researchers may don’t know what the effects of a clinical trial drug would be on a patient. As a safety precaution, researchers assess the blood platelet counts of trial participants frequently. If extreme adverse effects are discovered in a patient, he or she could be pulled out of the study.
As discussed earlier, thrombocytopenia is a medical disorder in which the blood has an abnormally low platelet count (lower than 150,000 platelets per microliter of blood). When medicines or drugs cause this disorder, it is known as drug-induced thrombocytopenia.
Researchers in clinical trials depend on analyzers to measure blood platelets. However, most analyzers overestimate the blood platelet count. Increasing the use of point of care treatment (POCT) full blood counters can help clinical researchers measure more accurate platelet counts.
Discover the automated CBC analyzer - Sight OLO
Disclaimer: The content of this knowledge post intends to provide general information related to topics that are relevant to blood diagnostics and may not be used in relation to the operation of Sight OLO. For detailed information on the diagnostic parameters and specifications of Sight OLO, please refer to the official Operator's Manual.