Point of Care Testing (POCT)
Definition, Comparisons, Devices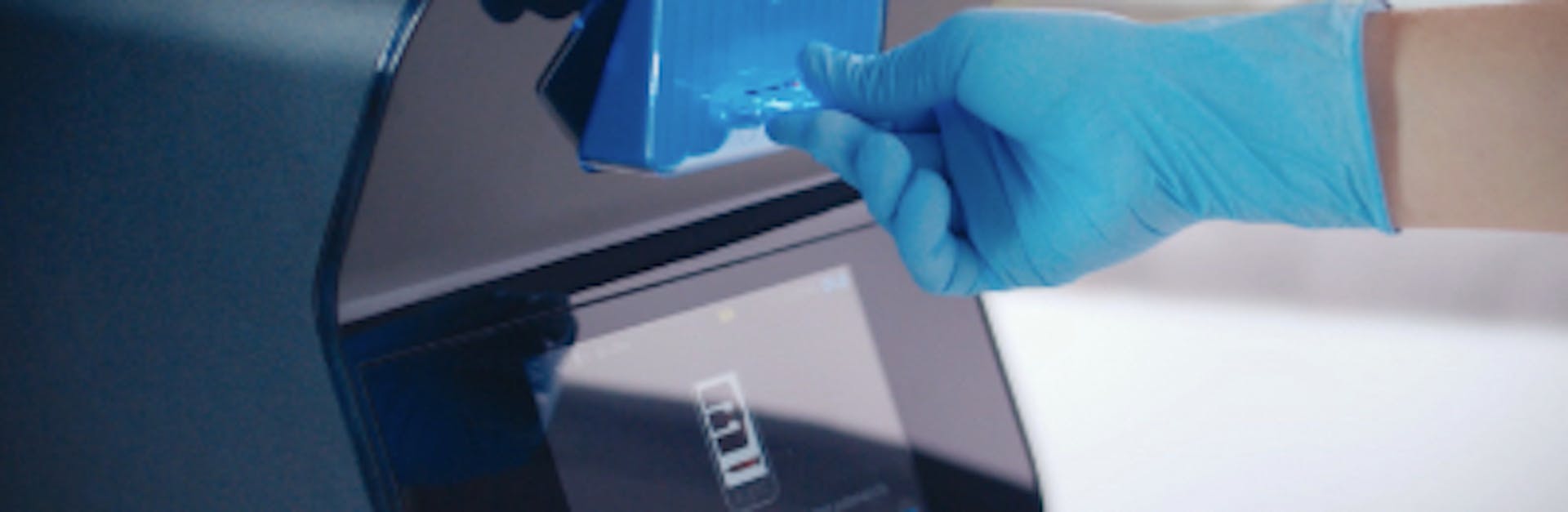
Providers of healthcare make efforts to treat patients quickly and to achieve the best possible outcome.
Quick and accurate test results can help to provide the best quality patient care and allow a health professional to make better and more effective decisions with their patient. Point-of-care testing, also known as near-patient testing, typically means carrying out a test using a device or test kit in the presence of the patient and without the need to send a sample to a laboratory.
Many new point-of-care devices utilize technological advancement to improve the quality of care.
What is point-of-care testing?
Point-of-care testing, often abbreviated to POC testing, is medical testing done at or near the point of care. In this context, POC refers to the location of the patient.
Sending all samples and specimens away to be processed at medical laboratories means waiting a long time for results. This can lead to wasted time in critical contexts or patients being treated without their care team having full information about their needs.
Instead, POC testing makes it far easier for results to be obtained quickly and reliably. With these results available, medical staff can more easily make informed decisions about a patient’s treatment and care.
POC testing vs. laboratory testing: Pros and cons
The main advantage of point-of-care testing is the shorter time it takes to obtain a result. Typically, results may also be presented in a way that is easier to understand, but this is not always the case and results may still require a healthcare professional to interpret them safely.
POC testing can also be performed by people who have not had formal laboratory training. This includes nurses, doctors, paramedics and testing by patients themselves. There are many kinds of near-patient testing, including malaria antigen testing, pregnancy tests, blood glucose monitoring, urinalysis and many more.
These tests often require relatively easy sample collection such as body fluids (e.g. saliva or urine) or finger-prick blood. Together with other portable medical equipment, such as thermometers or blood pressure devices, they can facilitate rapid and convenient medical assessment.
However, POC testing can have disadvantages. For example, based on the available technology used in the device, studies have shown that errors may be more frequent with POC testing than with laboratory testing. This can arise because the POC testing environment is generally less controlled than laboratory conditions and the results can be at higher risk of external interference than laboratory processes, which can lead to inaccuracy.
POC approaches can also be more costly than laboratory based testing. A study from 1995 demonstrated that the cost of POC testing for glucose was anywhere from 1.1 to 4.6 times higher than the same test in the laboratory. There are hidden costs that may often be overlooked, such as those associated with a quality control program or equipment upkeep. However, other kinds of hidden costs such as buildings, staff and overheads can apply to laboratory testing as well.
Nonetheless, the immediacy and convenience of POC testing can balance the increased costs. Rapid results can allow a treatment plan to be put into effect quickly, and where time is critical for better care, this can make a big difference.
Even where time is not critical and is more a matter of convenience, being able to move on with diagnosis and treatment is almost always of benefit to the patient. In some circumstances, a rapid result can help to allow a safe medical discharge from hospital, shortening the length of stay and helping to reduce costs of care. There are also examples of wearable monitoring and testing devices, which can decrease the rate of readmittance to hospital, by providing telemetry results to the clinic or information that patients themselves can use.
As technology continues to develop and point-of-care testing devices continue to improve, the issues of accuracy associated with POC testing are likely to resolve. As more experience and understanding is gained with using point-of-care devices, the benefits of quick results and ease of testing are likely to come to be seen as significant and desirable as well as routine.
Hematology point-of-care devices
Point-of-care testing has become popular in many medical subfields, including hematology. In recent years, continued progress in medical device engineering has resulted in more advanced POC testing devices.
Over the past several decades, the POC hemoglobin meter has been a popular and useful device. However, when compared with a laboratory complete blood count, this indicates only a small part of the useful or important information available from a full analysis of the blood cells.
More recently, the use of a range of techniques in combination with advanced digital technology has allowed the development of a point-of-care complete blood count analyzer. Among other approaches to achieve this, engineers have employed digital microscopy and machine vision using near‐infrared spectroscopy and multiple wavelength light absorption.
This means that the complete blood count can now be carried out as a point-of-care test with the same accuracy as traditional laboratory reports, with less invasive sample collection, greater speed and more convenience.
Complete blood counts are just one of many tests that POC testing devices are capable of. Other common hematology point-of-care testing devices include:
- Prothrombin time analyzers, for evaluating blood clots.
- aPTT testing, for hemostatic assessment.
- D-dimer testing, to rule out pulmonary embolism or DVT.
- Viscoelastic assays, for trauma and obstetrics.
- Activated clotting time testing, for monitoring heparin levels.
- Malarial antigen testing, for screening for malaria.
Today, the most commonly used and modern point-of-care testing devices have been shown to produce accurate and reliable hematology results, promoting better quality medical care across a wide range of conditions.
POCT for clinical trials and research
In recent years, researchers have integrated more advanced POCT devices in clinical trials to provide results faster than local laboratories.
Clinical trials often require that participants have specific characteristics. Some examples of clinical trial POCT include pregnancy, glucose, oxygen concentration, and flu tests. Researchers can verify the status of participants at the site of the clinical trial. POCT screening can rule out participants who do not fulfill the requirements of the study.
One major application of POCT testing in clinical trials is rapid CBC testing. Researchers can obtain quantitative CBC results in just a few minutes. Applications of rapid CBC testing in clinical trials include:
1. Identifying participants with anemia
A rapid CBC test typically includes red blood cell, hemoglobin, and hematocrit counts. If any of these are low, it could indicate that an individual has anemia. In clinical trials involving subjects with anemia, a rapid CBC test can quickly confirm the presence of the disorder.
2. Identifying participants with blood disorders
Just as in the case of anemia, other blood disorders can also be identified quickly using a rapid CBC test. Some disorders that can be discovered include autoimmune disorders, bone marrow disorders, leukemia, lymphoma, myeloproliferative neoplasms, myelodysplastic syndrome, sickle cell disease, thalassemia, and cancer that has spread to the bone marrow.
3. Screening for infections
In clinical trials to develop better treatment for immune disorders, a rapid CBC test can quickly identify participants with infections (high or low WBC count). This means that patients with infections can receive life-saving treatment quickly. If researchers discover infections at a rapid rate, then they can also find the root cause faster.
4. Monitoring patients’ reactions to clinical trial drugs (companion diagnostics)
Rapid CBC testing post-treatment can help monitor patients’ reactions to clinical trial drugs. With frequent CBC testing, researchers can quickly halt therapy if patients are experiencing extreme adverse effects. Frequent CBC testing can also improve patient adherence as it can uncover patients who are not correctly following the prescribed therapy.
A publication in Applied Clinical Trials highlighted three case studies of POCT for clinical trials and research:
1. Screen and enroll in a single visit
In an influenza study, researchers used a POCT device to test participants for influenza, get rapid results, and enroll them right away. The alternative would have been to let patients go home and wait for results from a lab before enrolling. Several of these patients may have fallen sick and not returned for enrollment.
2. Reduce screen failure rates
In a global chronic kidney disease clinical trial, researchers used a POCT device to pre-screen participants. They tested for estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (UACR).
3. Obtain faster results
In a rare disease study, scientists used a POCT device to measure C-Reactive Protein (CRP). The test enabled them to identify patients who were having “heart-attack-like” symptoms.
Discover Sight OLO - Near-patient Testing
Disclaimer: The content of this knowledge post intends to provide general information related to topics that are relevant to blood diagnostics and may not be used in relation to the operation of Sight OLO. For detailed information on the diagnostic parameters and specifications of Sight OLO, please refer to the official Operator's Manual.